Fecal incontinence, a condition where individuals cannot control their bowel movements, is often challenging and distressing for those affected. It can significantly impact one’s quality of life, resulting in embarrassment, social isolation, and a decline in mental well-being. Pelvic floor physiotherapy Sherwood Park offers a thorough and effective approach to managing and treating fecal incontinence. This therapy focuses on strengthening the pelvic health muscles, improving bowel control, and enhancing overall pelvic health.
How Pelvic Floor Strengthening Helps:
Pelvic floor strengthening focuses on exercises and techniques designed to enhance the strength, coordination, and endurance of the pelvic floor muscles. By improving the functionality of these muscles, individuals can gain better control over bowel movements and reduce instances of fecal incontinence.
Key Components of Pelvic Floor Physiotherapy:
Biofeedback:
This technique uses sensors to offer real-time feedback on muscle activity, aiding patients in learning how to control and strengthen their pelvic health muscles effectively.
- Surface Electromyography (sEMG): Small adhesive electrodes are placed on the skin near the anus or on a probe inserted into the rectum to detect electrical activity produced by muscle contractions. This muscle activity is then displayed on a monitor as visual or auditory signals, allowing patients to see and hear their muscle contractions in real time.
Pelvic Floor Exercises (Kegels):
Pelvic floor exercises, commonly known as Kegels, play a pivotal role in the management of fecal incontinence treatment. Pelvic floor physiotherapy in Sherwood Park suggests Kegel exercise that aims to strengthen the pelvic muscles, which are essential for maintaining continence and providing support to the pelvic organs.
Basic Kegel Exercises:
- Slow Contractions: Slowly contract the pelvic floor muscles as if attempting to halt the urine flow. Hold the contraction for 5-10 seconds, then rest for an equal duration. Repeat this exercise 10-15 times, aiming to progressively increase the hold duration as muscle strength improves.
- Quick Contractions: Perform rapid contraction and relaxation of the pelvic floor muscles. Perform this exercise 10-20 times in a row. This helps improve the muscles’ ability to react quickly and provide support during sudden increases in abdominal pressure, such as coughing or sneezing.
Bridge with Kegels:
A highly effective method for strengthening the pelvic floor muscles, glutes, and core involves lying on your back with knees bent and feet flat on the ground. Raise your hips to form a bridge position, and then squeeze and lift your pelvic floor muscles while holding the bridge. Maintain the contraction for 3-5 seconds before lowering your hips back to the starting position while relaxing your pelvic floor muscles. Repeat this process for ten repetitions three times a day. This combined movement not only targets the pelvic floor muscles but also enhances overall stability and strength in the glutes and core.
Electrical Stimulation:
Mild electrical impulses stimulate the pelvic floor muscles, promoting strength and coordination. This is particularly useful for individuals with significant muscle weakness.
- Transcutaneous Electrical Nerve Stimulation (TENS): Small surface electrodes are placed near the anal area, delivering mild electrical impulses to stimulate and strengthen pelvic floor muscles.
- Intravaginal or Intrarectal Electrical Stimulation: A specialized probe inserted into the vagina or rectum delivers direct electrical impulses to the pelvic floor muscles, enhancing strength and coordination.
- Neuromuscular Electrical Stimulation (NMES): Controlled electrical impulses cause pelvic floor muscles to contract and relax, supporting muscle re-education and rehabilitation.
Manual Therapy:
Physiotherapists may use hands-on techniques to release tension, improve blood flow, and enhance muscle function in the pelvic floor.
- Trigger Point Release: Physiotherapists apply direct pressure to particular points on the pelvic floor muscles to relieve tension and alleviate discomfort.
- Myofascial Release: Gentle, sustained pressure is used to stretch and release the connective tissue surrounding the pelvic floor muscles, improving flexibility and function.
- Soft Tissue Mobilization: Hands-on techniques manipulate the soft tissues of the pelvic floor to improve blood flow and reduce muscle tightness.
Bladder and Bowel Retraining:
This involves establishing regular bowel habits and dietary modifications to improve bowel function and reduce incontinence episodes.
- Scheduled Toileting: Patients are encouraged to follow a fixed schedule for bowel movements to train the body to empty at regular intervals.
- Stool Softening Strategies: Recommending over-the-counter stool softeners or natural remedies to ease bowel movements and prevent stool incontinence.
Lifestyle and Behavioral Modifications:
Physiotherapists provide advice on dietary changes, fluid intake, and bowel management strategies to support pelvic floor health.
- Dietary Adjustments: Physiotherapists recommend increasing fibre intake and incorporating a balanced diet to improve bowel regularity and consistency.
- Fluid Management: Guidance on proper fluid intake helps maintain hydration without overloading the bladder or bowels, promoting regular bowel movements.
Breaking the Taboo: Pelvic Floor Physiotherapy for All
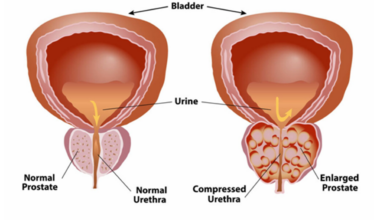
Many think that pelvic health physiotherapy is only for females, but men also face issues such as incontinence, pelvic pain, erectile dysfunction, and post-prostate surgery recovery. Consulting with a physiotherapist is essential for both men and women, as pelvic floor health is not a taboo topic. Male pelvic floor physiotherapy addresses specific issues like urinary incontinence, pelvic pain, erectile dysfunction, and recovery after prostate surgery. Female pelvic floor physiotherapy focuses on postpartum recovery, managing pelvic organ prolapse, urinary incontinence, pelvic pain, and pain during intercourse. Both men and women can benefit greatly from tailored pelvic floor therapies to improve their overall quality of life.
Restoring Daily Comfort and Well-Being:
Pelvic floor physiotherapy in Sherwood Park offers a comprehensive and effective approach to addressing fecal leakage through targeted pelvic floor strengthening techniques. Emerald Hils Physiotherapy in Sherwood Park not only enhances the strength and coordination of the pelvic floor muscles but also contributes to overall bowel health and quality of life. For individuals struggling with fecal incontinence, seeking the expertise of a specialized pelvic floor physiotherapist can lead to personalized treatment plans and successful management of their condition, ultimately restoring confidence and improving daily living.