Alzheimer’s disease is a complex neurodegenerative condition that affects millions of individuals worldwide. As researchers delve into the myriad factors contributing to its progression, the link between nutrition and cognitive health has come to the forefront. Adequate nutrition is needed for well-being, but it may also play a pivotal role in managing Alzheimer’s disease.
Moving beyond traditional medication, a multifaceted approach embracing diet could offer additional benefits to individuals grappling with this condition. Below, we delve into the intricate relationship between dietary habits and Alzheimer’s treatment, shedding light on the emerging nutritional strategies that could aid in managing symptoms and possibly slowing disease progression.
The Connection Between Alzheimer’s Disease and Nutrition
Evidence suggests that what we eat can influence brain health, with certain nutrients showing potential as protective agents against Alzheimer’s disease. The brain’s need for a steady supply of vitamins, minerals, and other nutrients to maintain cognitive function sets the stage for dietary interventions. Inadequate nutrition may exacerbate the neurodegenerative processes, highlighting the importance of a balanced diet in Alzheimer’s care.
Understanding this connection lays the groundwork for tailored nutritional strategies to support brain health. Living with Alzheimer’s can be incredibly challenging, not only for the patient but also for their loved ones.
Thankfully, there are numerous Alzheimer’s organizations dedicated to providing education and support to those affected by the disease. For those seeking more comprehensive information on the progression of Alzheimer’s disease and resources for support, a visit to alzinfo.org can provide valuable insights and guidance.
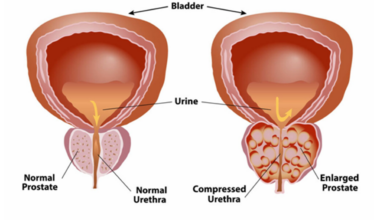
Additionally, the role of gut health in Alzheimer’s disease is becoming increasingly recognized. A healthy gut microbiome could influence brain health through the gut-brain axis, potentially affecting the disease’s development. This adds another layer to the complexity of dietary influences on Alzheimer’s, where prebiotics and probiotics might also play a role.
The Impact of Dietary Patterns on Alzheimer’s Progression
Longitudinal studies of dietary patterns have shed light on how lifelong eating habits may impact the risk and progression of Alzheimer’s disease. Diets high in saturated fats and sugars are often implicated as risk factors for cognitive decline. Conversely, patterns high in vegetables, fruits, fish, and unsaturated fats are associated with reduced risks, suggesting that diet does indeed play a critical role in brain health over time.
The antioxidants found in certain fruits and vegetables may protect neuronal integrity by combating oxidative stress, a known contributor to Alzheimer’s. Similarly, omega-3 fatty acids, prevalent in fish, are thought to have neuroprotective properties due to their anti-inflammatory effects.
These components can help support the structure and function of brain cells, potentially mitigating the impact of Alzheimer’s. While diet can influence risk and progression, it is not a cure or guaranteed preventive measure. Instead, dietary choices can be part of an integrative approach towards improving quality of life and possibly altering the disease’s trajectory.
See Also: Molecular Hydrogen Against Oxidative Stress
Addressing Nutritional Deficiencies
Recognizing and addressing nutritional deficiencies is vital for Alzheimer’s care. A comprehensive nutritional assessment can uncover specific deficiencies that may be affecting a patient’s cognitive health. Healthcare providers can then develop targeted dietary plans to correct these imbalances. Tailored nutrition interventions, in conjunction with medical treatment, might enhance the effectiveness of care plans for Alzheimer’s patients.
Supplementation can also be a part of addressing deficiencies, especially when dietary adjustments alone are insufficient. For example, vitamin D or B12 supplements may be needed for some individuals with Alzheimer’s who are unable to get enough from food sources. However, supplements should be used judiciously and always under the guidance of a healthcare provider to ensure they are safe and necessary.
Moreover, hydration is a commonly overlooked aspect of nutrition that can significantly affect cognitive function. Alzheimer’s patients can be at risk of dehydration, which can exacerbate symptoms of confusion and cognitive impairment. Caregivers and healthcare providers should monitor fluid intake to maintain hydration levels, integral to holistic Alzheimer’s care.
Overall, nutrition holds a critical place in the dialogue surrounding Alzheimer’s treatment, with a balanced diet rich in key nutrients offering potential benefits for cognitive health. Emphasizing the need for further research, we understand that how we nurture our bodies can intersect with medical interventions to foster a more robust defense against the effects of Alzheimer’s disease. Ultimately, dietary strategies, while not a panacea, are an essential part of holistic care for individuals facing this arduous journey.